What’s wrong with my knee?
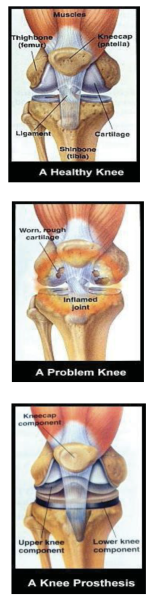
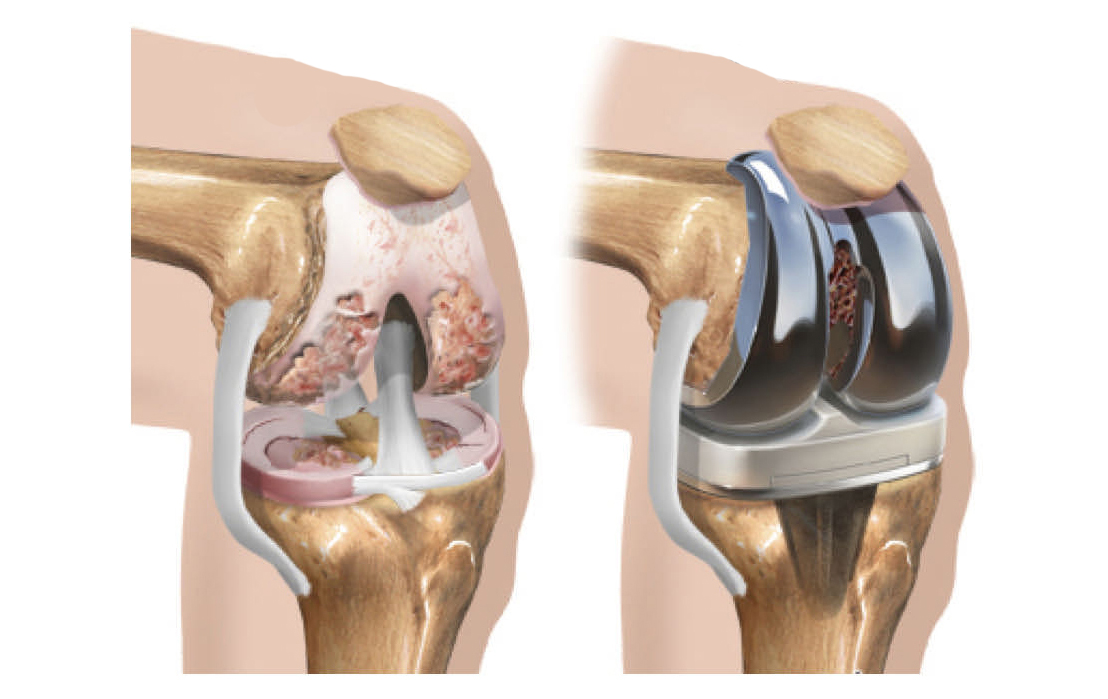
The knee is a hinge-like joint, formed where the thighbone, shinbone and kneecap meet. It is supported by muscles and ligaments and is lined with cushioning cartilage.
In Joint Replacement Surgery (Arthroplasty), the old joint is replaced with a new mechanical joint called a prosthesis.
A healthy knee joint bends easily. Cartilage, a smooth tissue, covers the ends of the thigh bone and shin bone and the underside of the knee cap. Healthy cartilage absorbs stress and allows the bones to glide freely over each other. Joint fluid lubricates the cartilage surfaces, making movement even easier.
A problem knee is stiff or painful. Cartilage cracks or wears away due to usage, inflammation or injury. Worn, roughened cartilage no longer allows the joint to glide freely, so it feels stiff. As more cartilage wears away, exposed bones rub together when the knee bends, causing pain. With time, bone surfaces also become rough, making pain worse.
A knee prosthesis lets your knee bend easily again. The roughened ends of the thigh bone and shin bone and the underside of the kneecap are replaced with metal and strong plastic components. With new smooth surfaces, the bones can once again glide freely. A knee prosthesis does have limitations, but it can let you walk and move with greater comfort.
What are some of the risks involved in having a total knee replacement?
We want you to understand the benefits and risks of joint replacement surgery. The ultimate goal is for you to regain function of your knee with minimal pain and discomfort. Most people recover smoothly from surgery. Just like any surgery, there are risks involved in having a joint replaced. Some risks are more specific to total joint replacement, and others are risks of any surgery. Most patients have no complications. However, it is important for you to understand the risks and possible complications of a total joint replacement.
Blood clots
- During and after surgery, your activity level will decrease, which causes your blood flow to slow down.
- This can lead to clotting of the blood in your legs, which could potentially travel to your lungs, heart, and brain.
- In order to prevent this complication, the following measures are helpful:
- Compression stockings, compression sleeves or foot pumps during surgery and after surgery to improve circulation
- Ankle pump exercises after surgery
- Blood thinner medication
- Getting out of bed several times each day to help circulate your blood flow, starting the day of surgery or the next day.
Even with the best care, it is still possible for blood clots to form. Therefore, it is important for you to know the signs and symptoms of blood clots and to let the medical staff know immediately if you are experiencing any of these symptoms:
- Swelling
- Redness
- Pain
- Tenderness and warmth in the calf or lower leg
Infection is a possibility with any surgery.
- Infection can occur at the incision site or internally, around the prosthesis. It is an uncommon risk, but it can be a potentially serious complication.
- You will be given antibiotics during and after your surgery to help prevent this complication from happening.
- If, however, infection around your prosthesis does occur, additional surgery may be needed to remove the infected prosthesis and replace it with a new one.
- After surgery, we ask for you to take prophylactic antibiotics for any dental procedure, surgery or other medical procedure that may increase your risk of infection in your blood stream that could travel to your prosthesis. Additional information about prophylactic antibiotics will be provided to you by your surgeon.
Dental injury
- During your surgery, teeth could be potentially loosened, chipped or dislodged. If this occurs, please let your anesthesiologist know.
Prosthetic loosening, wear and/or breakage
- After many years, your new prosthesis could potentially loosen from the bone or you may experience some wear of your prosthesis. If severe, surgery may be needed to revise the joint to make it more stable.
- It is extremely rare for a metal or plastic prosthesis to break. However, if it should occur, surgery would be needed to revise the joint.
Nerve injury
- Nerve or blood vessel injury may occur during surgery.
- This is very uncommon, but if it does occur, these nerves usually will improve or completely recover with time.
- Numbness on the outside part of your knee after a knee replacement is normal and will usually improve with time.
Reactions to anesthesia or pain medications
- Please let us know if you have experienced a reaction to anesthesia from a surgery in the past or to any pain medications taken in the past.
Blood loss and transfusion
- Our team tries to minimize your blood loss during surgery. However, there is a small chance you may need a blood transfusion during or after surgery. Your age, overall medical health and your post-operative blood levels will determine if you need a transfusion.
Loss of limb
Death
Before surgery you may be asked to attend and/or obtain the following:
- Medical Clearance
- Cardiac Clearance
- Other Clearance
- Dental Clearance
- Pre-op Physical Therapy Evaluation & Home Exercise Program Instructions
- Total Joint Class
- Pre-Admit Appointment
Medical and dental clearance
Knowing your overall health helps give you better and proper medical care while in surgery and during your hospital stay. Therefore, you may be requested to provide pertinent information about yourself from your medical doctor to better assist in that care. This may include EKG’s, blood work, cardiac stress test, pulmonary function test, etc.
Because the threat of infection is a major risk factor to joint replacement, we may also request dental information regarding the status of your teeth and gums. A silent or unknown infection in your mouth could travel through your bloodstream and cause infection around your prosthesis, which could be devastating to your new joint. This would require additional operations, hospital stay and lengthy use of antibiotics. If you have not seen a dentist in the last twelve months, we may request that you make an appointment for a dental exam prior to surgery.
Frequently Asked Questions
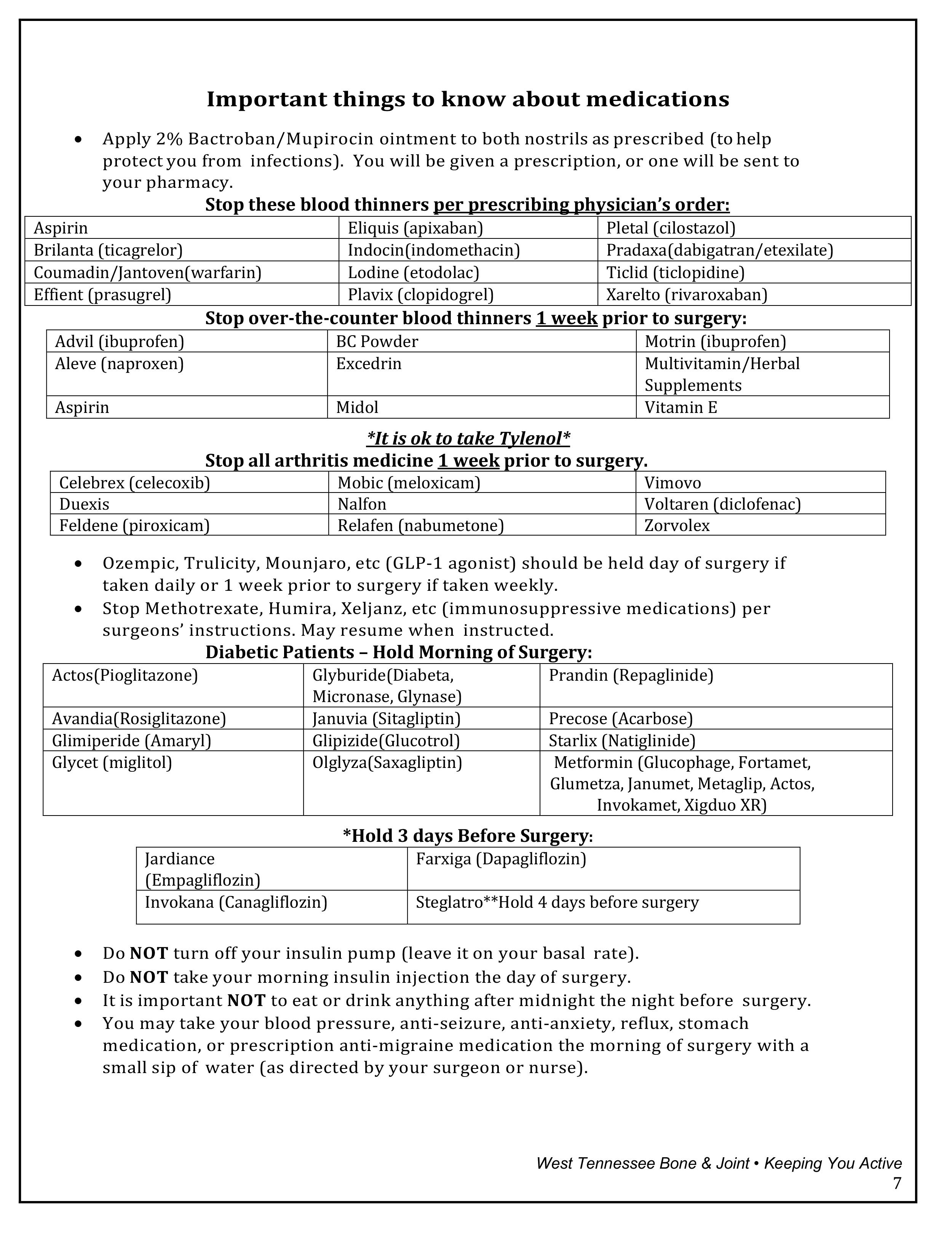
1. What about my daily medications before surgery?
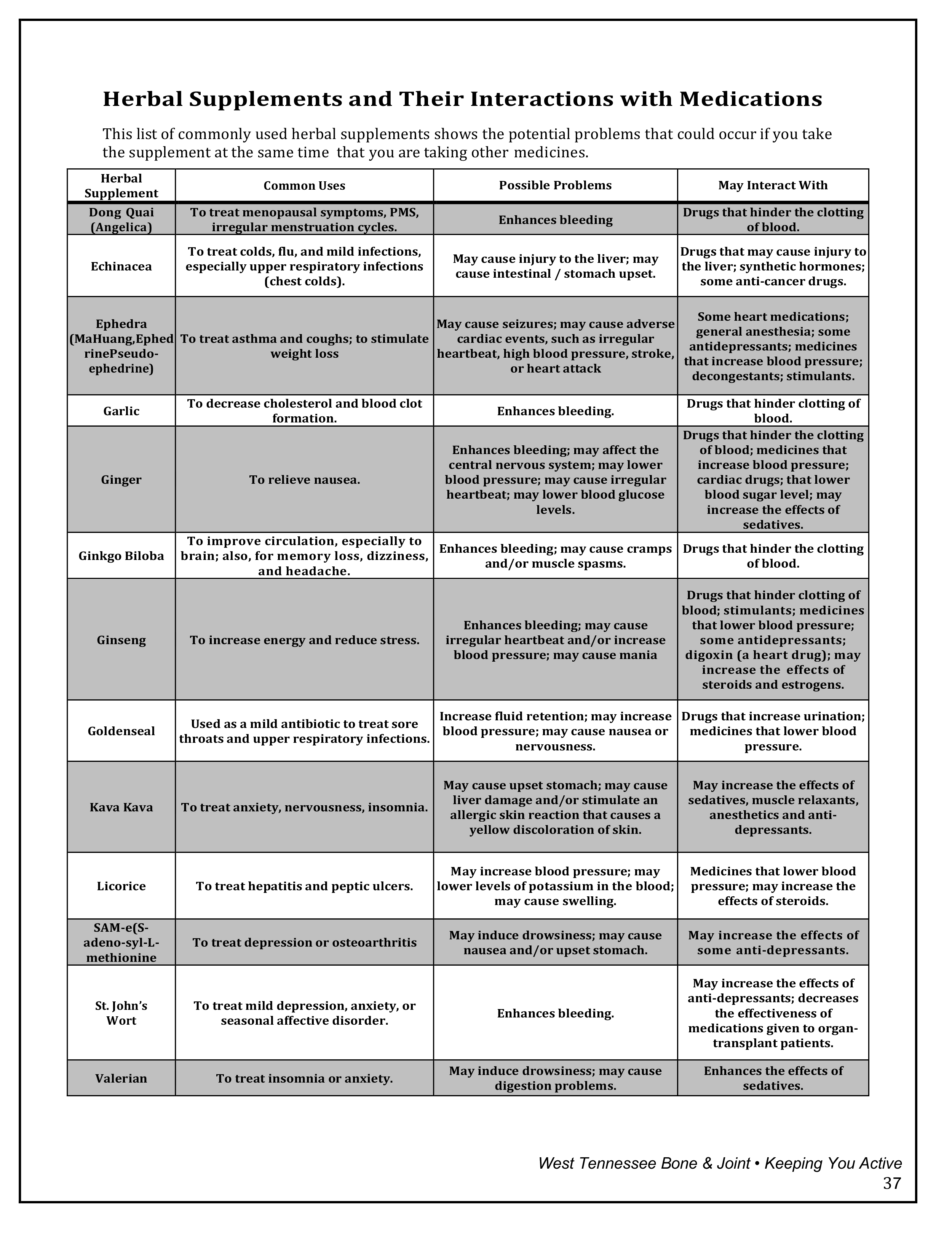
At the time of your pre-admission testing, the medications you routinely take will be reviewed with you. You will be advised to stop taking any medications before surgery, such as anti-inflammatory pills. You will also be told which medications to take the morning of surgery with a small sip of water. You will be given specific instructions about how soon before surgery you should stop taking blood thinning medications.
2. How long will I be in the hospital?
For joint replacement surgery, the majority of patients are able to go home the day of surgery.
3. What if I need extended care?
Your goal is to go home, as quickly and as safely as possible. However, a few patients are not yet capable of managing at home. Other arrangements may be made by your surgeon.
4. Will I have the opportunity to ask questions?
Questions and concerns will be addressed at the time of your visit with the surgeon. You will also have opportunities to ask questions during the time of your pre-admission testing. Also, feel free to call 731-661- 9825 (Jackson) or 731-644-0474 (Paris) for any further questions.
Positive approach to planning your total joint replacement
Preparing mentally for surgery is just as important for you and your family or support person, as it is for your surgeon and the rest of the medical team involved in your knee replacement procedure. Because of medical advancements, total joint replacement surgery should relieve your pain and discomfort and improve your activity level. It is important to remember that the pain and activity limitations after surgery will be different than what you are experiencing now, and that they will be short term. A significant portion of the recovery process is using your new joint by walking and doing the exercises that your doctor orders.
Depending on your condition, your recovery and exercise plan will be tailored to meet your needs. Each patient recovers differently, and joint replacement revisions often progress at a slower pace than the initial surgery.
It is important for you to make a commitment to follow your doctor’s instructions and work on your exercise plan after surgery in order to benefit most from the joint replacement. If you or your family need support coping with surgery and recovery—either physically or emotionally—please talk with the staff. The improved lifestyle after recovery is worth the risk and stress of surgery.
A significant portion of the recovery process is using your new joint by walking and doing the exercises that your doctor orders.
Prepare for your procedure
Start your checklists to prepare for your hospital visit
Your physician’s office may provide you with this manual in advance of your surgery. Please take time to read your manual, ask any questions, and make sure that you take care of the things that need to be done several days or weeks ahead of the surgery date. Surgery is your primary path toward getting yourself back to being the person you want to be—so don’t let any unnecessary delays stand in your way!
Attend a joint replacement therapy visit
You should schedule a therapy visit two to three weeks before surgery when possible. Ask your surgeon’s office how to schedule your pre-surgical PT evaluation visit or call 731-410 2357 – Jackson or 731-407- 4738 – Paris.
Making arrangements
Taking care of a few items now will help make your return home smoother and safer! As we have discussed, total joint replacement surgery can relieve the pain and discomfort of your arthritic joint. However, there is a six-to-eight-week recovery period after your surgery during which you will experience different types of pain and discomfort. During this recovery phase, you will be using your new joint according to the instructions given to you at discharge and by your physical therapist as directed by your physician. We ask you to stay committed to these instructions and to your exercise plan. However, there are some limitations and arrangements that need to be made prior to surgery to ensure an easier recovery afterward.
Transportation
- You will not be driving initially after surgery. Your surgeon will instruct you when it is safe to resume driving. This could be anywhere from 1 to 6 weeks post-operatively.
- You may need to find someone to drive you to therapy and to your doctor’s appointments.
- You may also need someone to pick up groceries, medicines, etc.
Work
Arrange to be off work approximately 12 weeks, although you may be able to return sooner. The exact length of time will be determined by your doctor at your six-week post-surgical appointment. At that time, your doctor will consider your recovery rate and type of work you perform.
Prepare your home for your return
Kitchen
- Move most frequently used items to the counter so you can reach them without bending over or climbing (food, skillet, utensils, dish-washing items).
- Freeze meals or schedule to have a friend bring you meals for 4-6 weeks.
- You may find it helpful to stock up on prepared foods such as canned, boxed or frozen foods.
- Check to see if your local grocery store will deliver orders to you.
Bedroom
- If your bedroom is on the second floor, get creative!
- Your doctor may initially limit your trips up the stairs to only once a day after surgery.
- Find a space on the first floor to call your own for the first couple of weeks.
- Stock this area with things you need for the day, so you can rest.
Bathroom
- Put non-skid material in the bathtub or shower.
- You may want to purchase a tub transfer bench or shower stool if you have a tub shower.
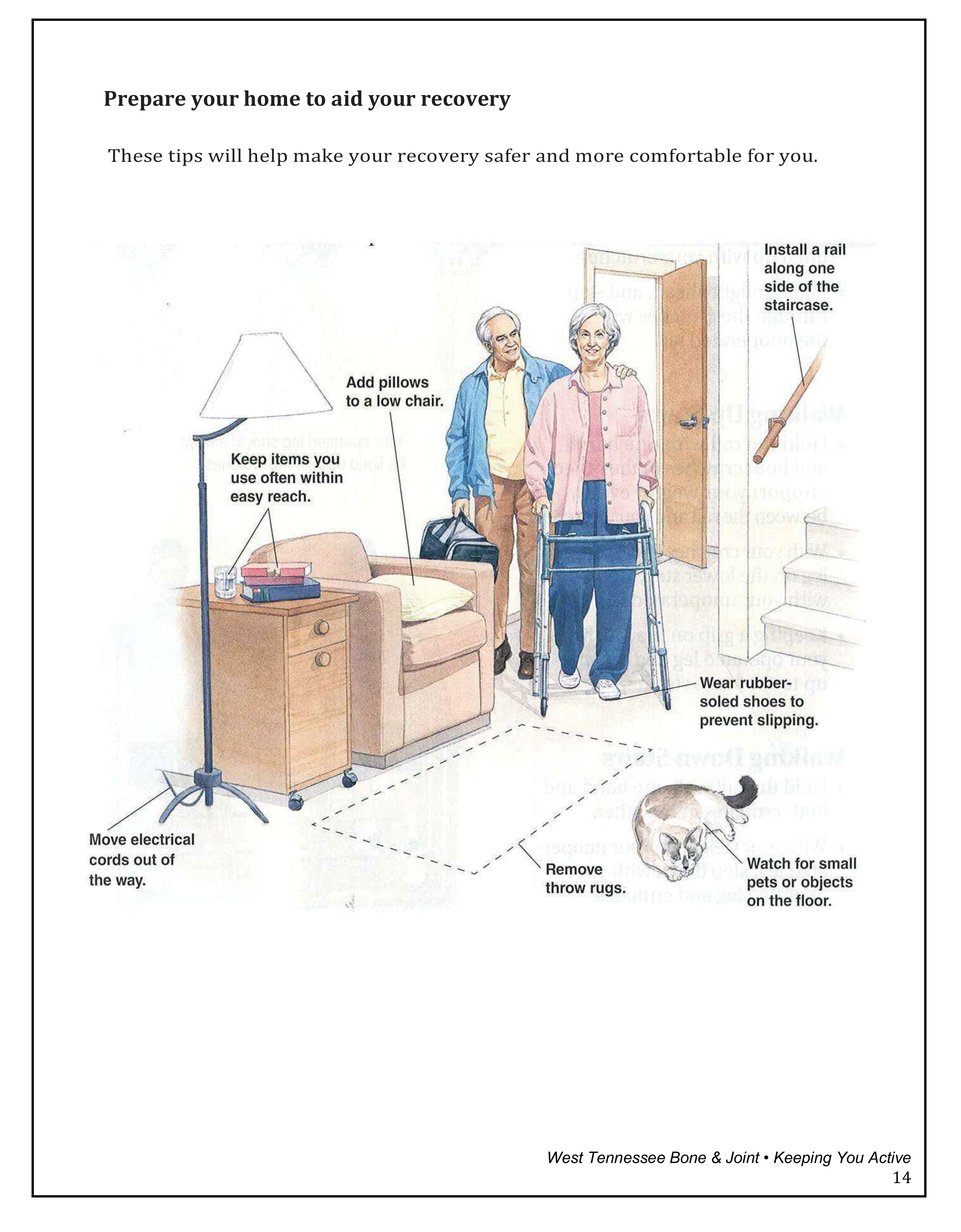
“Fall-proof” your home
- Remove all throw rugs.
- Imagine using a walker and check for “trouble spots” in your home before your surgery.
- Check rooms for small objects, cords or stools that could cause tripping.
- Use a rolling cart to move items around and to keep them within easy reach.
- After surgery, use your prescribed walking aid at all times. Change positions slowly and avoid rushing to prevent loss of balance.
Other tips
- Rearrange your most frequently used items to a convenient level, somewhere between your waist and shoulder.
- Place a phone within easy reach wherever you are.
- Make sure that you have good lighting and that the light switch is within easy reach.
- Use a cushion to raise the seat in a low chair.

Help prevent infection…
- Taking a bath or shower is recommended the night before or morning of surgery.
- Do not apply lotion to the area where surgery is to be performed.
- In the hospital and at home, performing proper hand hygiene is essential.
- Wash your hands before eating and after using the rest room.
- Wash your hands after petting your animal(s).
Your defenses may be down after surgery, which is normal. Any step you can take to prevent infection is a step in the right direction.
In the hospital or at home, performing proper hand hygiene is essential.
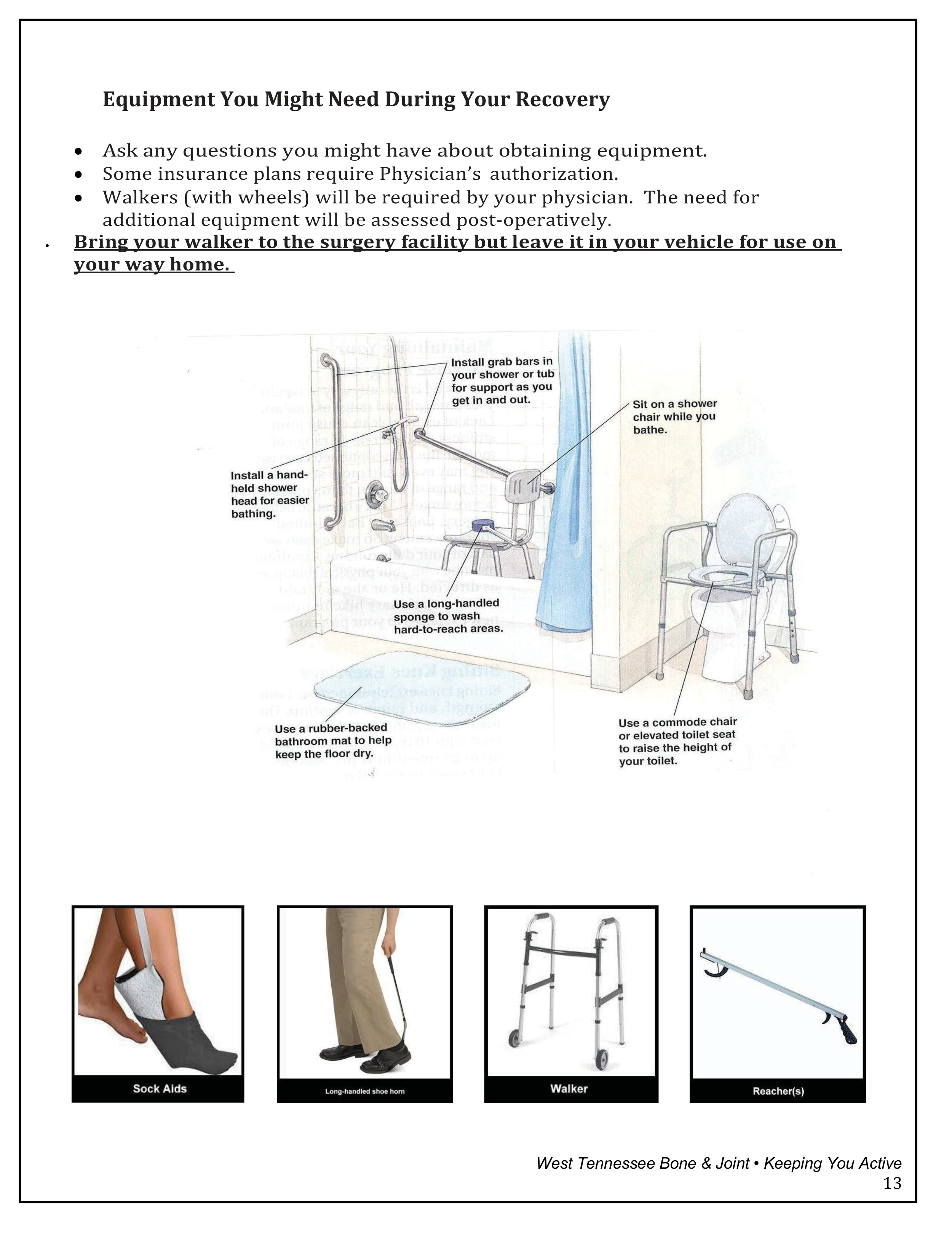
Equipment you might need during your recovery
- Ask any questions you might have about obtaining equipment.
- Some insurance plans require a physician’s authorization.
- Walkers (with wheels) will be required by your physician. The need for additional equipment will be assessed post-operatively.
- Bring your walker to the surgery facility, but leave it in your vehicle for use on your way home.
Prepare your home to aid your recovery
The friends’ and family’s role in your recovery
Your family and friends are very important in helping you during your recovery.
Examples of ways they can help you prepare:
- Stock up on canned and frozen or packaged food.
- Move your most frequently used items (such as food, skillet, extra toilet paper, soap, etc.) to cabinets between your waist and shoulder level, helping you avoid reaching and bending.
- Prepare a room for yourself with all the needed supplies so that you can rest during the day.
- Remove rugs and other clutter for safe walking.
- Run errands, grocery shop and drive you to follow-up doctor’s appointments.
- Arrange for your caregiver (Coach) to attend at least one of your therapy sessions in the hospital after surgery.
What should I bring? What should I leave at home?
What should I bring to the surgery facility?
- Eyeglasses or contact lenses with case
- Loose-fitting shorts and T-shirts
- Rubber sole shoes
- Dentures, hearing aids, prostheses
- Any special equipment, including walker (leave in vehicle), and other daily activity aids, as applicable
- Your driver’s license and insurance/Medicare card
- A list of all medications you are currently taking. Please include dosage and instructions. Also, include over-the-counter medications and herbal supplements
- A caregiver (Coach), who should be with you in the hospital to be part of your care team, when possible.
What should I leave at home?
- Cigarettes and all tobacco products
- Jewelry, remove all body piercings
- Credit cards
- Large sums of money (anything more than $5)
- Keys
What else should I know?
- Do not eat, chew gum, or suck on or eat mints, drink or smoke after midnight the night before your surgery unless instructed to do so by your physician. You may brush your teeth and rinse with mouthwash. Your physician highly recommends you stop smoking/use of nicotine four weeks prior to surgery.
- Take any medicines as directed the morning of surgery with a small sip of water.
- If diabetic, check with your primary care physician about how to adjust your diabetes medication.
- Please leave your belongings (like your suitcase and walker) in your car until your room has been assigned.
- Surgery usually lasts one-two hours.
- During your surgery, your family will be free to visit the cafeteria or other designated areas. Someone from surgery will contact them either on their cell phone or a hospital-assigned phone. Your surgeon will contact them after the surgery is complete.
- Narcotics may cause constipation. You are already prone to constipation because of surgery and lack of exercise. Increasing fiber intake while on narcotics may be a necessity. Over the counter stool softeners are available at your local drug store (i.e. Dulcolax, MiraLAX, etc.).
- It is important for you to breathe deeply to help your lungs clear and avoid complications, such as pneumonia. Bed rest, drowsiness, anesthesia and pain often keep you from taking normal deep breaths. Make use of the incentive spirometer you are given in the hospital and remember to use it.
Day of discharge: going home after knee replacement
Once you are stable enough to be discharged, you will go home. The majority of patients go home the day of surgery. Most patients will travel by car driven by a family member or friend. Please make these transportation arrangements before coming to the hospital for surgery. Insurances will not cover ambulance transportation to your home.
Discharge instructions
Discharge is a busy time. You will be given therapy if you have not met your goals. You will be given the following by the orthopedic nurses:
- Prescriptions for pain medicine as ordered by your doctor
- Instructions on medications to resume at home
- Your doctor may prescribe medication to prevent blood clots from forming, such as Aspirin, or prescription anticoagulants/blood thinners.
- Instructions on how to take care of yourself
- Instructions on when and where your staples or stitches will be removed
- If your appointments have already been made, these will be reviewed with you.
- We request that you call your surgeon’s office and verify your follow-up appointment with the physician who performed your surgery.
If there is any information that you do not understand, please ask the staff before you leave.
“Call Us First “(1-888-661-9825 –Jackson Office) (1-866-470-2663 – Paris Office) if you have:
- Increased redness, bleeding, pain or swelling on or around your incision
- Fever higher than 101◦ or as specified by your doctor
- Change in color or amount of drainage more than seven days after surgery
- Shortness of breath and/or chest pain, seek immediate attention at an emergency room
- Any other questions or concerns
Activity after surgery
Follow the activity guidelines and exercises as instructed by your doctor or physical therapist. Always ice your knee after any extended activity or exercise.
Walking
- Use your walker or crutches while walking.
- As your muscles get stronger and your walking progresses, your therapist will instruct you to progress to a cane and then to no assistive device. These progressions should only be made if you can continue walking without a limp. If you are limping, please return to the previous device.
- Goal: While at home, try to walk for 5 minutes every hour you are awake to keep your joint from getting stiff. You can gradually increase this time, but make sure to allow for rest and ice between activities.
Sitting
- Do not sit for longer than 30 minutes at a time. Get up, walk and change positions.
- On long car trips, stop at 30-minute intervals. Get out and move around. With the lack of movement, your knee may become stiff or swollen, and you are more prone to blood clots.
- If resting in recliners, be sure your knee is not bent, and your lower leg is properly elevated with a pillow under your ankle. The reclining position does not aide circulation or help reduce swelling.
- Occasionally throughout the day, rest with your heel elevated on a surface opposite you to work on getting your knee straight.
- Whenever resting, put ice on your knee.
Swelling
- Swelling is common after surgery. Typically swelling occurs in your thigh, knee, ankle and foot.
- To decrease swelling, lie with your foot elevated above your heart while icing. This can be done during rest periods throughout the day.
- The more you ice, the more quickly the swelling will come out of your knee, which will make therapy easier.
- Remember to ice all sides of your knee.
- Ice can be done with your Iceman, frozen ice bags, frozen peas, frozen Karo syrup or your favorite method. Always place a thin layer between the ice and your skin. TED hose work as a great barrier.
- Iceman: if you choose to rent or purchase the Iceman, place a thin barrier (i.e., small hand towel) between your knee and the ice machine bladder to prevent frost bite.
- Ice therapy sessions should be 20 minutes on, 20 minutes off throughout the day (recommended by the manufacturer). This type of constant icing is essential to get the inflammation and swelling down so that the healing process can begin.
Dressing
- When putting on pants or shorts, always put the surgical limb in first.
TED hose
- Use TED/compression hose as prescribed by your physician.
Stairs
- If you need to use stairs, we recommend making one trip up and down each day. Be careful and hold onto a railing or another person for support when using stairs.
Sports
- DO NOT participate in sports during the first three months after your surgery.
- DO NOT use whirlpools, spas, or swimming pools until you doctor tells you it is okay.
- DO NOT use weight machines for the first three months after your surgery.
- You may eventually resume some sports that do not put your knee at risk, such as golfing, swimming, bicycling, yoga and dance.
Sleeping
- Avoid sleeping on your side until your doctor tells you it is okay.
- If (when) you sleep on your side, sleep on your non-operative side, placing a pillow between your knees for comfort.
- Avoid every type of waterbed.
- DO NOT place a pillow under your knee when sleeping on your back.
Resuming sexual activity
- It is generally safe to resume sexual activity as soon as you feel able.
Driving
- DO NOT drive until your doctor tells you it is okay.
The facts about pain management
During and immediately following your surgery, you will receive pain medication by injections or through the IV. As you begin to recover from your surgery, you will be switched to oral pain medication. If you receive a femoral nerve block before surgery, your pain should be much more tolerable for the first 12 to 24 hours.
What will be your goal for pain control?
Some degree of pain is unavoidable. While you are in the hospital, you will be receiving pain medication to help control pain. It is important to tell your nurse if you are having pain. Don’t wait until the pain is severe. The more severe the pain, the harder it is to control. We will try to reduce your pain without compromising your ability to move, breathe deeply, or care for yourself.
Your nurse will ask you to rate your pain. A pain scale helps you rate your pain intensity. In the scale, 0 means no pain, and 10 is the worst pain possible. We cannot relieve all your pain, and you may feel some pain even with medications. However, we should be able to reduce it to a level of five or less. Be sure to mention if the pain suddenly increases or changes.
Important points:
- You will NOT be totally pain free.
- Pain medication is usually taken regularly. Don’t try to be a “hero” and wait too long or skip a scheduled dose in the first day or two after surgery.
- The longer you wait to take pain medicine, the worse your pain will become, taking longer to get under control.
- Contact your doctor’s nurse if your pain medication is not working or if you don’t like the way it makes you feel.
- Unrelieved pain robs your energy and takes away important time you could spend working towards a faster recovery.
- Your surgeon will prescribe pain medication to keep you comfortable. With strict federal laws regarding opioid use, it is important that you only take these medications as prescribed.
Some other things you can do to try to control your pain.
- Watching TV
- Changing positions
- Reading a book
- Listening to relaxation tapes
- Find out what works best for you
Equipment
- Compression Stockings: If ordered, they should be worn every day for the first three to six weeks. They help reduce swelling.
- Compression Sleeves/Foot pumps: These devices are used to help reduce the risk of blood clots in your lower legs.
- Knee immobilizer: If ordered, it should be worn while standing until a straight leg raise can be performed.
- Dr. Chandler (Only) – Knee immobilizer – wear knee brace only when sleeping for 6 weeks
- Cooling device: This device helps to reduce swelling. Please use as directed.
Physical therapy pre-op visit
Please call 2 weeks before surgery date. (If you live out of town, try to schedule this on the same day as lab work.) Please call for an appointment.
West Tennessee Bone & Joint Clinic – Main
24 Physicians Drive, Jackson, TN 38305
731-410-2357
West Tennessee Bone & Joint Clinic – Paris
1006 Cornerstone Drive, Paris, TN 38242
731-407-4738
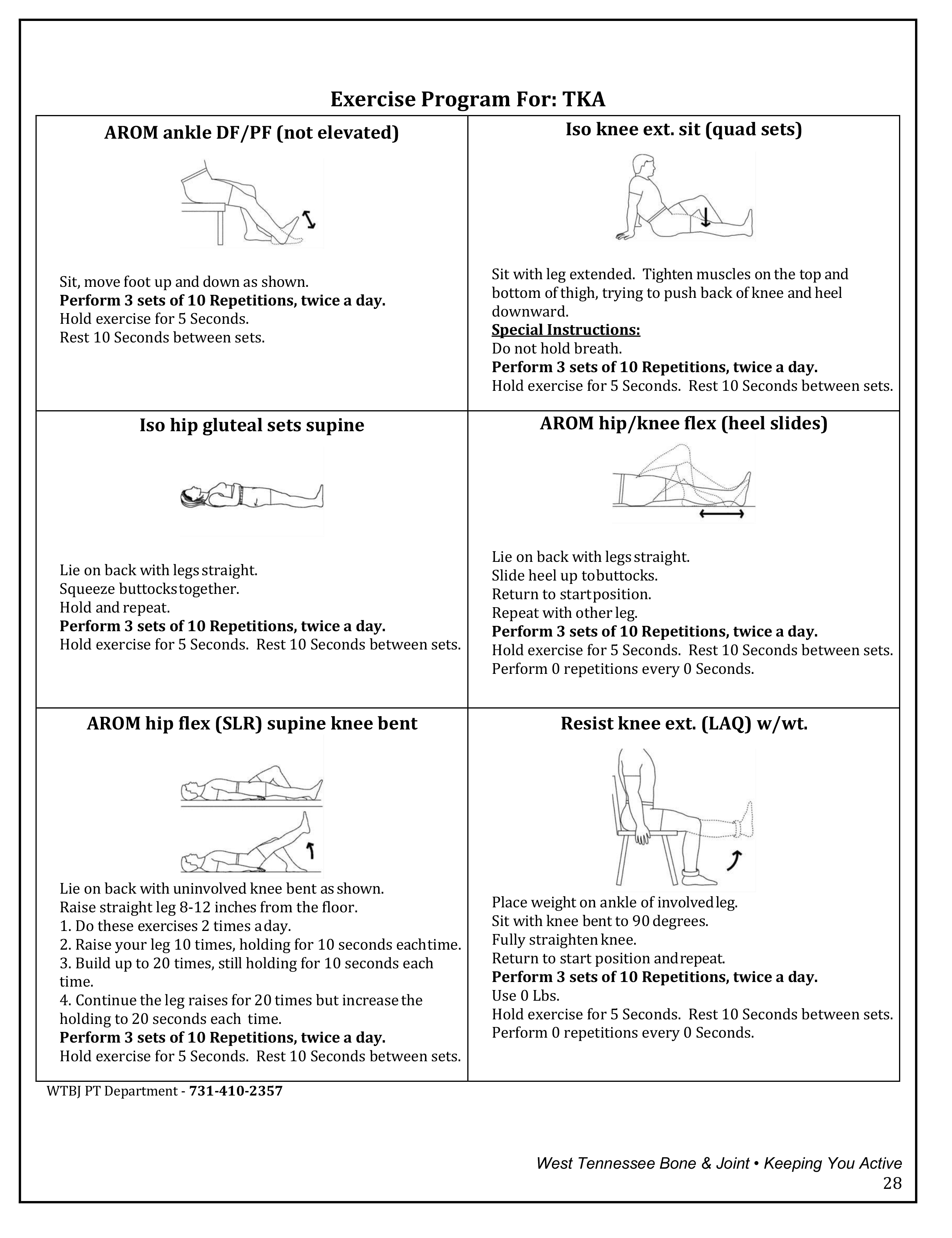
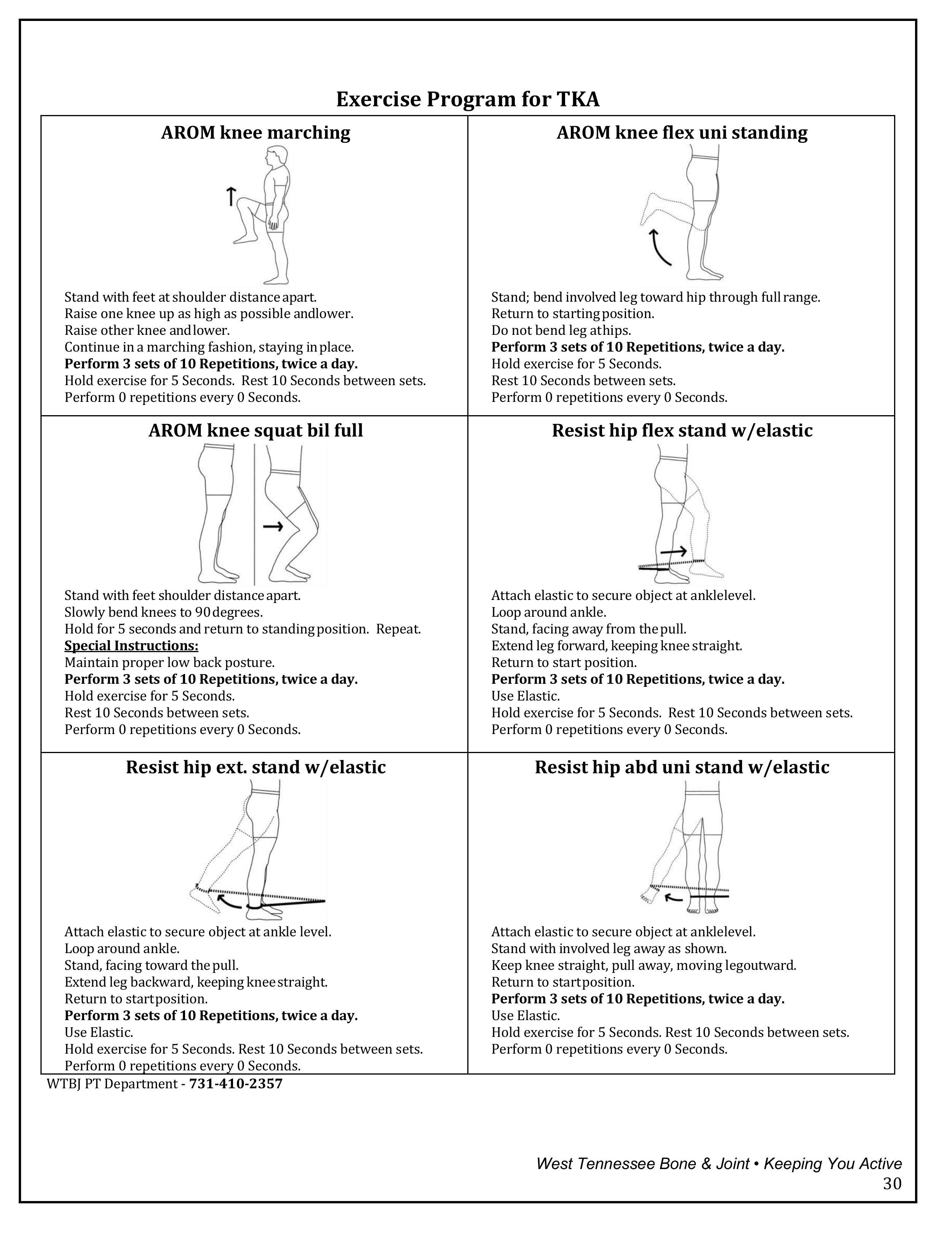
- Exercises will be issued to you by the Physical Therapist at your pre-op visit.
- Physical therapy will focus on improving your knee motion. Our goal for you at six weeks is to be able to straighten your knee to 0° of extension and bend your knee to 120° of flexion. Your physical therapist should be focusing on this during your therapy session. Once you gain your motion, strengthening can be started, but no heavy weights should be used until 3 months post-op.
- Physical therapy exercises should be performed twice a day. If you attend physical therapy that day, then you just need to perform another set of exercises on your own during the day. If you do not attend physical therapy, then you have two sets of exercises to perform that day.
- It is important that you attend your therapy visits. Therapy is a very important part towards your total joint healing.

Physical therapy total knee arthroplasty protocol
Goals:
- AROM 0°-120°, do not exceed 120° PROM
- Ambulate without an assistive device and without an antalgic gait/limp
- Climb stairs in a reciprocal pattern (one foot over the other) without upper extremities unless needed for safety
- Full functional mobility
Phase I (post-op day 4 to week 3):
- Physical Therapy 3x a week for 4 to 6 weeks. Follow up with surgeon at 3 weeks.
- Wear TED hose as directed by your surgeon/nurse. Remove at night. Wear for 3-6 weeks.
- Use ice at night, and during day when resting. ICE FREQUENTLY! Elevate legs with ankle pumps and ice to decrease excessive swelling.
- Progress from rolling walker to a straight cane when ambulating with equal weight shift, adequate balance for safety, and no excessive swelling of joint.
- Wound Care:
- Patient may shower when discharged from the hospital. Pat dry and follow the discharge nurse’s instructions on dressings. No lotion or ointments. NO soaking in bath.
- If staples are present, they will be removed at 3 weeks, and then steri-strips applied.
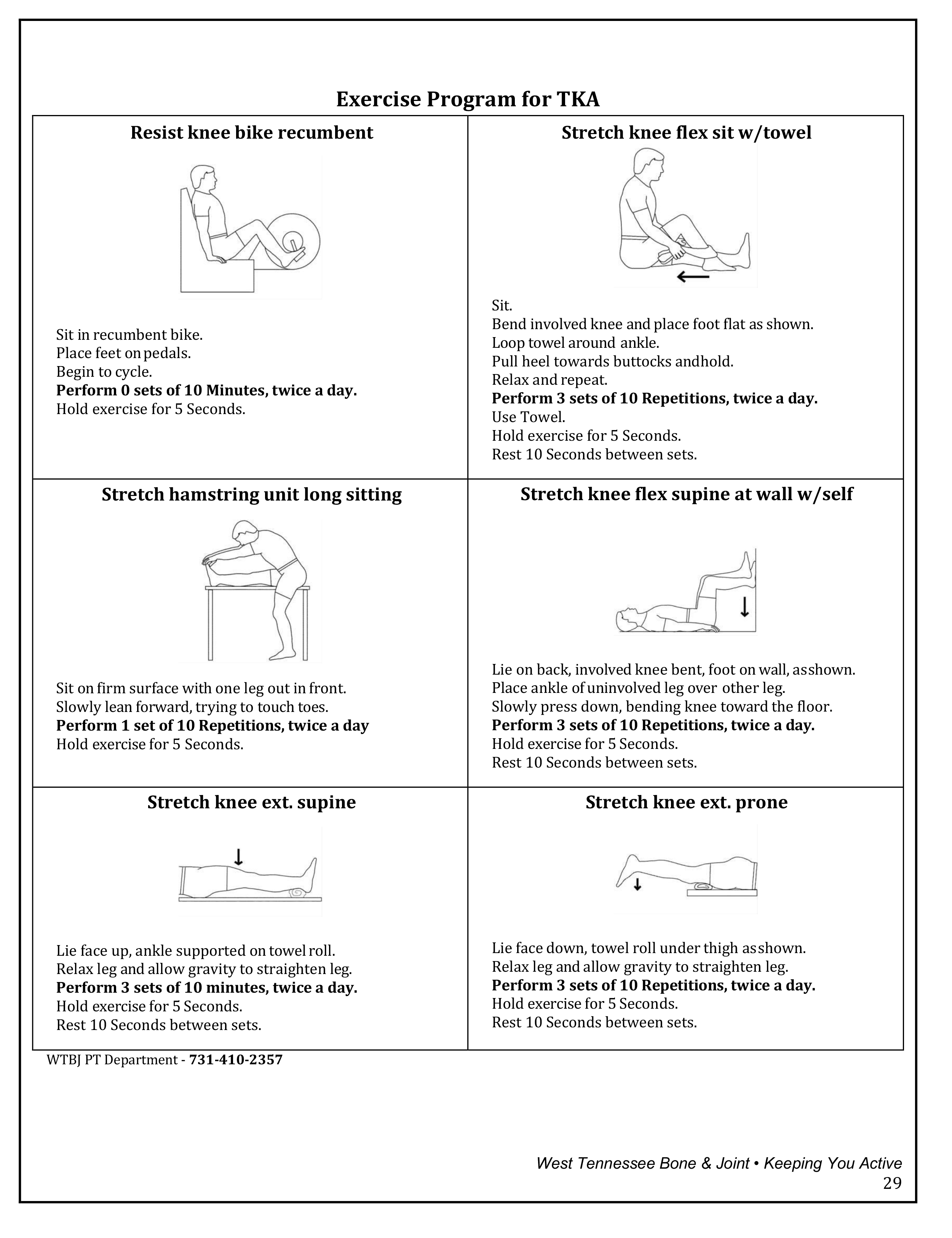
- Warm Up: Bike X 10 minutes. Only use moist heat over soft tissue musculature not at the joint line.
- AAROM at least 5°- 100°, use strap or belt for overpressure with heel slides.
- Mat Exercises/ HEP: quad sets, glut sets, heel slides active and with overpressure, SAQ, SLR, SL SLR, LAQ, and HS stretch. Knee Extension most important motion! Use NMES/Russian if needed for quad/VMO activation. If an extension lag is present, no cuff weights should be used.
- Patient to do HEP 2x/day
- Patient to ambulate home ~ 5 minutes/hour to increase circulation.
- Standing Exercises: calf raise, toe raise, marching, HS curls and mini squats. If patient progressing well with ROM, the initiate step ups 4”-6”.
- No weight machines
- Ultrasound can be used to decrease edema/pain and increase ROM. Settings for US: Freq: 3.3 MHz, 50% duty cycle, output 1.5-2.0 w/cm2.
- Manual therapy: patella mobilization, no distraction. Grade I-II PA/AP tibial mobs to decrease pain and increase mobility.
- No driving for 6 weeks with right knee, 4-6 weeks with left knee.
Phase II (week 4 – week 6):
- AROM 0°-120°
- Progress from SC cane to no assistive devise when patient able to ambulate safely and without a limp.
- Progress mat exercises: add up to 2# cuff weight to increase strength/difficulty, no > 2#, if patient receives pain, decrease or remove weight.
- Continue HEP 2X/ day
- Limit walking if patient does not have AROM 0°-120°.
- Progress standing exercises: add airex to exercises to increase proprioception, TKE with TheraBand, increase step height to 8,” eccentric step down 4,” SLS, wobble board, hip circuit, wall-sits, and sit to stand without UE. Exercise goal to increase ROM, strength, balance, proprioception, and function.
- Manual therapy: Grade I-II tibial mobs to decrease pain and increase ROM. Fibular AP/PA mobs to decrease risk of ITB tendonitis.
- NO weight machines!
- Begin scar massage with Vitamin E oil 6 weeks after surgery, unless your provider states otherwise.
Phase III (week 7 to 3 months):
- Continue with home exercise program from your physical therapist 4x a week to continue to gain strength, stability, mobility, endurance, and function. Able to use up to 5-pound cuff weights with mat exercises.
- Begin daily walks, starting with ¼ mile and gradually increasing. If swelling occurs, use ice to decrease.
- Climb stairs in a reciprocal pattern (one foot over the other)
- Able to begin upper body weight machines, only if you are sitting. NO leg weight machines!
- For endurance: walk outside, walk on track, water exercise, ride a stationary/recumbent bike, NuStep or elliptical machine; NO treadmill because of the compression on the new joint.
- Golf: May begin chipping/ putting at 6 weeks, may begin driving at 3 months. As with all activities, begin slowly and work yourself up to a full round.
Phase IV (3 months – years):
- Continue to do isolated knee strengthening exercises/home exercise program 3-4x a week.
- Able to use leg weight machines with low weight and gradually increase.
- Recommended Activities:
- Elliptical trainers
- Stationary/recumbent bike
- Walking
- Water aerobics or swimming
- Low impact aerobics
- Yoga, Tai Chi, Swill Ball exercise—some positions may need to be altered if loading the joint in flexion.
- Activities NOT Recommended:
- Running/jogging
- High impact aerobics
- Jumping rope/plyometrics
If you have any other questions, please contact our Physical Therapy team at 731-410-2357 or your surgeons’ nurses at 731-661-9825.
Preventing post-op infection
You have undergone a total joint replacement procedure. There are instances when infection in one part of the body may cause bacteria to circulate in your blood, possibly resulting in infection at the site of your implant. Therefore, it is essential you seek prompt treatment of infections anywhere in your body.

Good dental hygiene is important. You should see your dentist for regular dental care whether you are having a dental problem or not. Prompt treatment of any kind is important, including dental procedures such as the following:
- Dental extraction
- Periodontal procedures including surgery, sub-gingival placement of fibers/strips, scaling and root planning, probing, recall maintenance
- Dental implant placement and re-implantation of avulsed teeth
- Root canal instrumentation or surety only beyond apex initial placement of the orthodontic bands but not brackets
- Intraligamentary local anesthetic injections
- Prophylactic cleaning of teeth or implants where bleeding is anticipated.
Recommendations for antibiotic therapy from the American Association of Orthopaedic Surgeons are the following:
- Patients not allergic to Penicillin: Cephalex, Cephradine, or Amoxicillin 2 grams orally one hour prior to any dental or invasive procedure
- Patients not allergic to Penicillin and unable to take oral medications: Cefazolin 1 gram or Ampicillin 2 grams IM/IV one hour prior to any dental or invasive procedure
- Patients allergic to Penicillin: Clindamycin 600 mg orally one hour prior to any dental or other invasive procedure
- Patients allergic to Penicillin and unable to take oral medications: Clindamycin 600 mg IM/IV one hour prior to any dental or other invasive procedure.
No second dose is recommended for any of these dosing regimens.
The avoidance of bacterial contamination and infection should help reduce the risk of infection at the site of the total joint implant. Since prompt treatment is essential, please do not hesitate to consult your personal physician, your dentist or your surgeon should such a situation arise.
Concerns about addiction
You are taking narcotics because you hurt. When your pain from surgery decreases, your need for the pain medicine will decrease. The fears you or your family may have about addiction could:
- Prevent you from taking pain medicine
- Result in your “holding off” as much as possible between doses
- Result in taking lower doses of pain medicine when you still hurt.
All these result in needless suffering. Talk to the staff if you have concerns or fears about pain medication, a history of drug abuse, sensitivity to pain medication or low tolerance to pain.
Facts about addiction
- Addiction rarely happens in patients taking pain medicine to relieve postoperative pain (fewer, than 1% of patients).
- Most people are able to reduce or stop pain medicine when the pain decreases or disappears.
Taking pain medicine at home
- You will be given a prescription for pain medication.
- Plan ahead if you are getting low on pain medication. You may find it difficult to refill your prescriptions for pain medications during weekends, evenings or holidays.
- Within a few weeks, most patients can take Aleve® or Tylenol® for occasional pain. If, you’re still having a lot of pain at that time, it is important to discuss this with your surgeon.
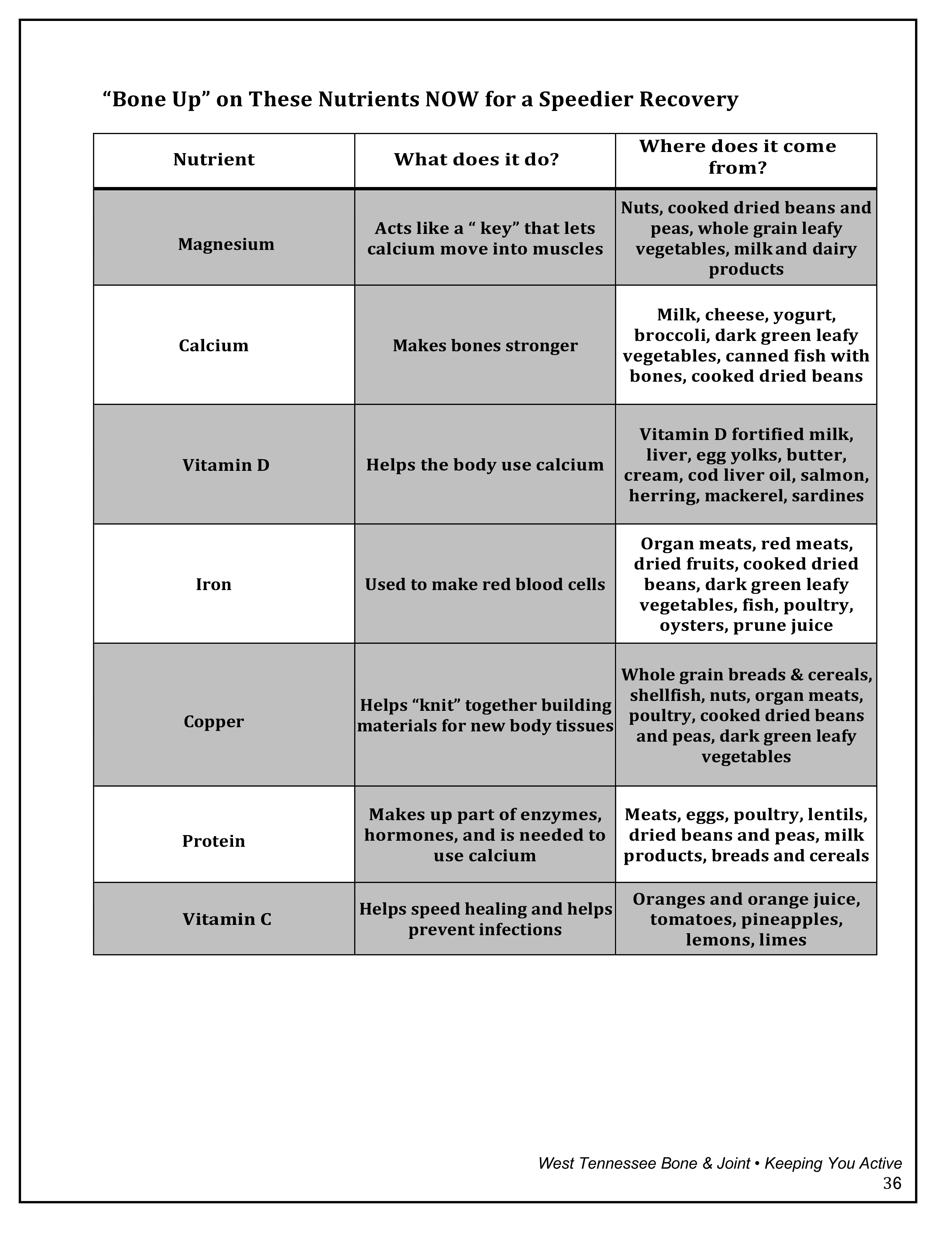
Orthopedic nutrition

Nutrition plays an important role in your recovery from orthopedic surgery. Assuring optimum nutrient intake will speed up the healing process by providing the building blocks for tissue repair and growth. This will help you get back on your feet as soon as possible. It will also help minimize any complications such as infection.
Try to increase the variety of foods in your diet during this time in order to capture these vitamins, minerals and trace elements. Your body has an increased need for these foods after surgery. If you desire to receive any information about modified diets or if you have any questions regarding proper nutrition, you can request a Registered Dietitian to come see you while you are in the hospital.
The following are general guidelines to help meet these needs. Try to follow these guidelines for six-eight weeks after your surgery during the healing phase.
The Food Pyramid
Eating well is important to your health and your recovery. The USDA’S MyPyramid is your personal guide to healthy eating and physical activity.

Download and print: checklist prior to surgery
Download and print: questions to ask
Reference numbers
Facilities/pre-admissions
Jackson-Madison County General Hospital
620 Skyline Drive, Jackson, TN 38301
731-541-6919
Jackson-Madison County General Hospital — North
367 Hospital Blvd, Jackson, TN 38305
731-541-6919
Physicians Surgery Center
207 Stonebridge Blvd, Jackson, TN 38305
731-661-6340
Henry County Medical Center
301 Tyson Avenue, Paris, TN 3824
731-642-1220
Physical therapy/rehab facilities
West Tennessee Bone & Joint Clinic – Main
24 Physicians Drive, Jackson, TN 38305
731-410-2357
West Tennessee Bone & Joint Clinic – Paris
1006 Cornerstone Drive, Paris, TN 38242
731-407-4738